ACL injuries are among the most typical knee injuries, especially to athletes and others who engage in physically demanding activities. The ACL, is one of the major ligaments in the knee that is responsible for holding the knee firm while one is trying to make sudden stops, jumping, or changing direction. Injury to this ligament can be frustrating as it causes pain, swelling, and instability in the affected area if torn. Anterior cruciate ligament reconstruction is one of the most used procedures for treating the knee and preventing further problems. The common treatment for the injury is surgery where the doctor replaces the damaged ACL with a graft.
What Are ACL Grafts?
ACL graft refers to the body tissue used to repair the knee joint that has experienced severe ligament damage. This graft forms the base upon which new tissues develop and form a functional ligament. There are many types of ACL grafts used by surgeons depending on the patient’s need, the extent of the activity, and the surgeon’s choice. The decision of an ACL graft is crucial to get the best results and resume normal activities. The main categories of ACL grafts are autografts (surgically taken from the patient’s body), allografts (donor tissue), and synthetic grafts.
Types of ACL Grafts
When it comes to ACL reconstruction, there are three primary types of ACL grafts:
-
Autograft
These grafts are autografts, meaning they are harvested from the patient’s body; usually the hamstrings, patellar tendon, foot/ankle tendon (Peroneous longus) and Quadriceps tendon (full/partial thickness). Many surgeons regard autografts as the best method of reconstructing the ACL as this tissue has a high success rate and is rarely rejected by the body.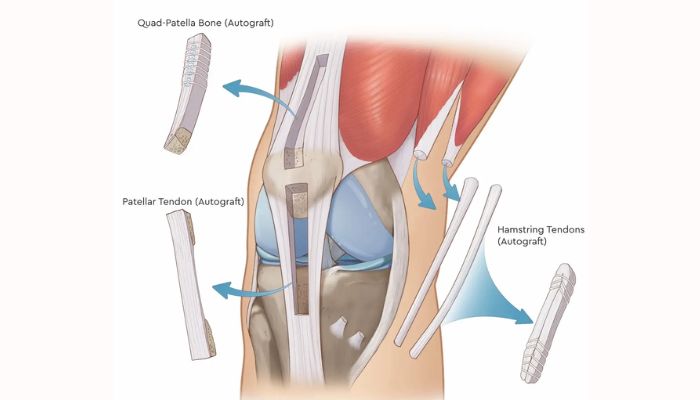
-
Allografts
These grafts are taken from a donor. Patients can be given allografts in case patients do not want to go through the process of harvesting the tissue from the patient’s own body, or autografts have been utilised in previous surgeries.
-
Synthetic Grafts
Autografts are relatively less frequent; however, such patients may still qualify for artificial grafts. Surgical meshes are created using synthetic materials that will act as ligaments.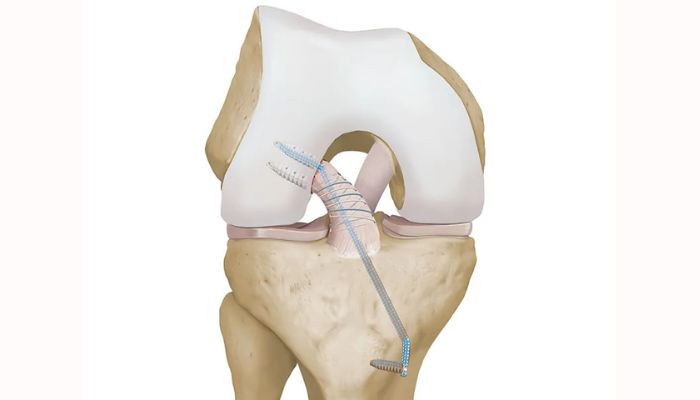
-
Allografts: Donor Tissues
Allografts are collected from donors, treated, and used as implants in the ACL reconstruction operations. This type of graft has become popular over the years because of some benefits, especially for those who are old or have lower activity levels.
Advantages of Allografts
- Less Invasive: In addition, allografts are taken from a donor instead of the patient’s body tissue, which makes the surgery less invasive and causes less pain and a shorter time to recovery.
- Good for Revision Surgeries: Allografts are commonly used in revision surgeries because the initial ACL reconstruction procedure was unsuccessful or because treating the patient requires bone spur from previous ACL surgery.
Disadvantages of Allografts
- Risk of Disease Transmission: It is possible to pass disease from the donor to the patient, even though there are various tests conducted on the donor.
- Longer Integration Time: The graft is often taken from a different part of the patient’s body, therefore it may take longer time to mesh with the knee of the patient than with autografts hence a longer time to heal.
-
Synthetic Grafts: Artificial Alternatives
ACL is reconstructed with synthetic grafts that are substitutes for the naturally occurring ACL. These grafts were once preferred more than the newer ones since they have a higher failure rate. Nevertheless, modern technology has prompted the use of synthetic grafts again depending on the nature of the case.
Advantages of Synthetic Grafts
- No Donor Needed: Synthetic grafts refined this plan by keeping away from the use of donor tissue hence wiping out the scandal of transmitting diseases and having to seek tissue removal.
- Immediate Availability: Allografts on the other hand require processing and have limitations concerning their availability, while synthetic grafts are procured immediately; they are also flexible.
Disadvantages of Synthetic Grafts
- Higher Failure Rates: Earlier, synthetic grafts were identified to have higher failure incidence than autografts and allografts. This has been made better by modern materials but the risk is a little higher.
- Potential for Inflammation: Synthetic materials may initiate inflammation or other immune-related reactions that prolong the healing period.
-
Hamstrings Autograft
The hamstrings autograft involves using the semitendinosus and, in some cases, the gracilis tendon from the patient’s leg. These tendons are folded and prepared to create a strong, multi-strand graft to replace the damaged ACL. This type of graft is popular due to its strength, flexibility, and minimal pain at the donor site. However, it may slightly weaken the hamstring muscles, which can affect certain athletic activities. It is a preferred option for patients who prioritize a less painful donor site and need a graft with a high success rate.
-
Bone-Patellar Tendon-Bone (BPTB) Autograft
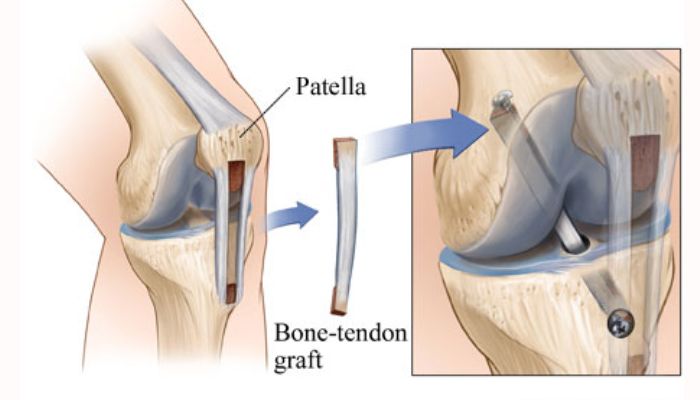
-
Central Quad Tendon / Superficial Quad Tendon Autograft
This option uses a segment of the quadriceps tendon, either from its central part or the superficial layer, with or without a bone plug from the patella. The quadriceps tendon provides a large and strong graft, suitable for patients with larger frames or those who have previously used other donor sites. It causes less discomfort during kneeling compared to the BPTB graft. However, harvesting this graft can lead to temporary quadriceps muscle weakness, delaying recovery. It is an excellent choice for patients who need a robust graft but want to avoid significant donor site morbidity.
-
Peroneus Longus Tendon Autograft
The peroneus longus tendon autograft is a newer technique that utilizes the tendon from the lateral part of the lower leg. This tendon is harvested through a small incision near the ankle and prepared as the ACL graft. It provides strong and flexible tissue while minimizing functional impact on the harvested site. Additionally, the peroneus longus tendon is relatively redundant, meaning its removal has minimal effect on lower leg stability. While it is an effective alternative to traditional grafts, long-term outcomes are still being studied, making it a promising option for patients seeking an innovative and less invasive solution.
Also Read: When Can I Run After ACL Surgery?
Pros and Cons of Each Type of ACL Graft
When deciding on the best type of ACL graft, it’s essential to weigh the pros and cons of each option.
| Graft Type | Pros | Cons |
| Autograft | High success rate, low rejection risk | Longer recovery time due to tissue harvesting, Morbidity at graft harvest site |
| Allograft | Less invasive, faster recovery | Small risk of disease transmission, slower integration, Availability issues |
| Synthetic Graft | Immediate availability, no donor needed | Higher failure rates, the potential for inflammation |
How to Choose the Right ACL Graft?
The factors responsible for the selection of the best types of ACL grafts are:
- Age: The younger and more active patients could benefit from autografts as they have lower failure rates compared to allograft executions. The elderly or patients with low activity levels might benefit from allografts since they have faster rehabilitation time.
- Activity Level: Those in high-impact sports or who need the best quality preference chose autografts since they are durable. The decision to opt for allografts may be relevant for patients not involved in intense physical work. Also, higher activity level patients may benefit from supplementation with synthetic graft options.
- Surgical History: People who previously had ACL surgery may need an allograft or synthetic graft options to avoid sacrificing the tissue somewhere else in their body.
- Surgeon’s Expertise: Some surgeons may prefer certain types of grafts since this is what they have used most often and achieved better results with.
- Patient Preference: Some patients might have their individual choices for any reason, pain, the time required to recover from the procedure, or use of the tissue from other people or synthetic materials.
Conclusion
ACL reconstruction is important to anyone who wants a fully functional return that will enable that person to regain his or her normal routine after an ACL injury. Such types of ACL grafts can be autografts, allografts, and synthetic grafts. Each has its benefits and drawbacks. The young and physically active patient uses autografts while for the patient seeking a less invasive surgery, allografts would be preferable due to a faster healing period. In certain cases, synthetic grafts are a possibility although it increases the risk rate. Therefore, it is the decision made based on factors such as; age, level of physical activity, and the choice of the respective surgeon. Therefore, open discussion with your surgeon is the best way through which your surgeon will advise you on the best types of ACL grafts for reconstruction surgery.